Central Nervous System (CNS)
- Primary Brain Tumors
- Secondary Brain Tumors (Brain Metastasis)
- Primary Spinal Cord Tumors
Primary Brain Tumors
Primary brain tumors originate from any cell type in the brain. In fact, there are over 120 different types of primary brain tumors. Tumors arising from glial cells (Gliomas) are the most common primary brain tumors affecting approximately 30 per 100,000 people in the United States. Most primary brain tumors are benign, but they can cause damage or death by invading or compressing nearby normal brain tissue. There are also malignant, or cancerous brain tumors. Primary brain tumors are treated with observation, surgery, surgery and radiation after surgery, or radiation alone. The choice of treatment depends on the type of brain tumor, the location of the brain tumor and the symptoms the tumor is causing the patient or the loss of function that may result if the tumor continues to grow. Brain tumors are as much individuals as are brain tumor patients and the treatment for each individual patient is personalized according to that patient’s circumstances. The individual treatment recommended is best decided in a team approach including the neurosurgeon, radiation oncologist, medical oncologist and often a physical therapist, a psychologist and a social worker.
Gliomas arise from the “supporting cells” that are believed to support and nourish the nerve cells which perform the functions of thinking, controlling muscle movement and other functions essential to life. Astrocytes give rise to the most common type of gliomas, the astrocytomas. Astrocytomas themselves can be classified according to grade from I-IV. Grade typically correlates with the aggressiveness of the tumor. Typically Grades 1 and 2 astrocytomas are slow growing tumors and may be present for years before they cause problems for the patient. Grade III astrocytomas are called anaplastic astrocytomas and have a much more aggressive behavior and always require treatment. Grade IV astrocytomas are also called Glioblastomas or Glioblastoma Multiforme. Glioblastomas are an extremely aggressive form of brain tumor that usually follows a rapid growth behavior and invades and destroys a large portion of the surrounding normal brain. These tumors are ideally treated with maximal safe surgery which is followed by a combination of daily radiation treatments combined with chemotherapy. New “targeted agent” therapy is showing promise as an alternative or as an addition to standard chemotherapy.
Other types of gliomas include ependymomas, which arise from the lining of the cavities within the brain which contain the cerebrospinal fluid. These include anaplastic ependymoma, myxopapillary ependymoma, and subependymoma. Another type of glioma is the oligodendroglioma and this type includes oligodendroglioma, anaplastic oligodendroglioma, and anaplastic oligoastrocytoma. These types of gliomas are quite rare and a detailed discussion is not appropriate here, but is best held between a patient with this type of diagnosis and the physicians who will be treating this patient.
Other primary brain tumor types include tumors arising from the brain coverings or meninges (meningiomas) and supporting tissues such as blood vessels (Hemangiomas) or abnormal connections between arteries and veins (Arteriovenous malformations) which could rupture and bleed, white blood cells (Lymphomas), nerves (Neurinomas), pituitary gland (Pituitary Adenomas) and pineal gland (Pinealomas or ).
Brain tumors are invasive and grow in a limited space within the skull by directly damaging (invading) adjacent parts of the brain as well as taking up space by their growth and putting pressure on all of the brain. Because of their location, treatment should often not be delayed. Occasionally, brain tumors in non-critical areas which grow very slowly may simply be observed and followed with imaging such as CT or MRI and clinical visits with the patient to observe for evidence of tumor progression either based on the patient’s symptoms or by growth on scans.
Conventional MRI is the most effective imaging modality in the work-up of CNS tumors because MRI usually gives the most detailed picture about the extent of the tumor. Depending on the type of tumor, the tumor’s location, the rate of growth of the tumor with the resulting damage to nearby structures or the causation of symptoms for the patient, surgery is often recommended as the initial treatment. Radiation therapy may be recommended in some circumstances after the surgery or occasionally as the primary treatment of brain tumors. In some cases, chemotherapy may be recommended in addition to radiation therapy:
• Radiation can be given after surgery for residual disease.
• Radiation may be the preferred treatment when a low-grade glioma has been diagnosed in a critical area of the brain that cannot be surgically removed, and therapy is felt to be necessary.
• Radiosurgery is an emerging modality of treatment that can be used either for cure, pretreatment or salvage after conventional radiation
Secondary Brain Tumors or Brain metastases.
Brain Metastases
Metastasis is a word that simply means “spread”. So brain metastases are cancers that originated somewhere in the body outside the brain and have “spread” by the blood to lodge in the brain where the metastases (tumors that have spread) grow and damage the normal nearby brain. Any tumor can spread to the brain, but the most common tumors to do so are lung cancer, breast cancer, colorectal cancer, pancreatic cancer, kidney cancer, bladder cancer and melanoma. Lung cancer, the leading cause of cancer deaths in the United States, and breast cancer, the most common cancer in women, are responsible for more than half of the cases of brain metastases in the United States. Metastases to the brain may be single, meaning there is one tumor, or multiple meaning that there are two or more tumors that have spread to the brain. It is estimated that well more than 100,000 new cases of brain metastases occur in the United States each year.
Brain metastases are special because of the blood brain barrier. The blood brain barrier is unique, because it prevents many types of toxic chemical from reaching the brain, and this includes most types of chemotherapy. So any cancer cell that is able to slip through the blood brain barrier and into the brain itself is completely protected from the chemotherapy and may multiply to form a tumor which can damage the normal brain and cause symptoms. The symptoms caused by brain metastases depend on the area of the brain where the metastasis is located and what body functions that area of the brain controls. Common symptoms of brain metastases include headache from brain swelling, dizziness, weakness of a specific body part, poor coordination, problems with thinking or memory and possibly seizures.
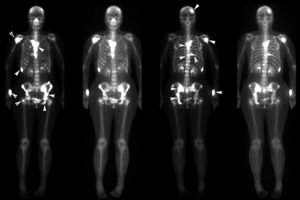
Depending on several factors including the age and health of the patient, the type of cancer that has spread to the brain, the size and location(s) of the tumors within the brain, and the number of tumors possible treatments include surgery and post-operative radiation, or radiation alone either with whole brain radiation or with stereotactic radiosurgery. Stereotactic radiosurgery involves focusing high doses of radiation exactly on the metastases. Most commonly, stereotactic radiosurgery is given as a single large dose of radiation, but sometimes this can be given with a few separate treatments. This has the advantage of sparing much of the normal brain tissue from the effects of radiation and providing the best chances of long term control of the metastases. Recent studies have demonstrated that selected patients with 3 or fewer brain metastases may have improved tumor control and survival compared to patients receiving conventional whole brain radiotherapy.
Each case of brain metastases is unique. The expected duration of treatment and any side-effects of treatment must be discussed in detail with the physician who will be delivering the treatments.
Primary Spinal Cord Tumors
Tumors that begin in the spinal cord (primary spinal cord tumors) are very rare and occur in about 1 per 100,000 people. Metastatic cancer (secondary cancer or cancer that has spread to the spine from elsewhere) is far more common. Because these primary spinal cord tumors are so rare, very few clinical trials have been performed to determine in a systematic manner the best treatment of these tumors. As such, doctors use a “best common sense” approach and custom tailor the treatment to each patient as best suits his or her needs.
In the broadest of terms, primary spinal cord tumors can be divided into 2 groups. Tumors arising from the covering of the spinal cord or from nerves coming off the spinal cord. These include meningiomas, schwannomas, and neurofibromas. The other type of primary spinal cord tumor arises from cells making up the spinal cord itself. These include astrocytomas, ependymomas, hemangioblastomas and lipomas. There are other types of primary spinal cord tumors, but these are the most common of these overall very rare tumors.
The spinal cord is best thought of as an interstate highway that nerve impulses (traffic) uses to connect the brain and the rest of the body. This is a two-way street. Impulses come from the brain to the body to control muscle action, and from the body to the brain to carry touch sensations. Primary spinal cord tumors can affect either lane of traffic, and often affects both. Initial symptoms of primary spinal cord tumors reflect interference with this traffic. This includes interference with the brains ability to cause muscles to move resulting in muscle weakness and problems with walking and balance or possibly loss of control of the bowel or bladder. Likewise, interference with touch sensations traveling to the brain usually results in numbness but can also result in unusual sensations or even pain.
Because of the risk of damaging the spine and disrupting this essential traffic, surgery is difficult at best, and carries a high risk of damage to the flow of nerve impulses. Because of this risk of severe collateral damage, surgery, and sometimes even biopsy, cannot be safely performed. In those cases, the treatment of choice is radiation. In certain cases, chemotherapy may also be used along with radiation.
Unfortunately, the spinal cord has a maximum safe dose of radiation that can be given as treatment. Often, this safe dose of radiation, about 25 treatments, is not enough to gain long term control of the tumor. Eventually, tumors that have received maximum safe doses of radiation may begin to grow again. In these cases, additional radiation is not possible without high risk of damage to the spinal cord. Chemotherapy is an option to slow down tumor growth in cases where maximum safe doses of radiation have been given.